The Expanding Role of Remote Triage
Remote triage has become one of the most important tools for modern healthcare delivery. Large scale health systems such as Veterans Affairs manage millions of patients, each with diverse needs, and must ensure timely access to safe advice.
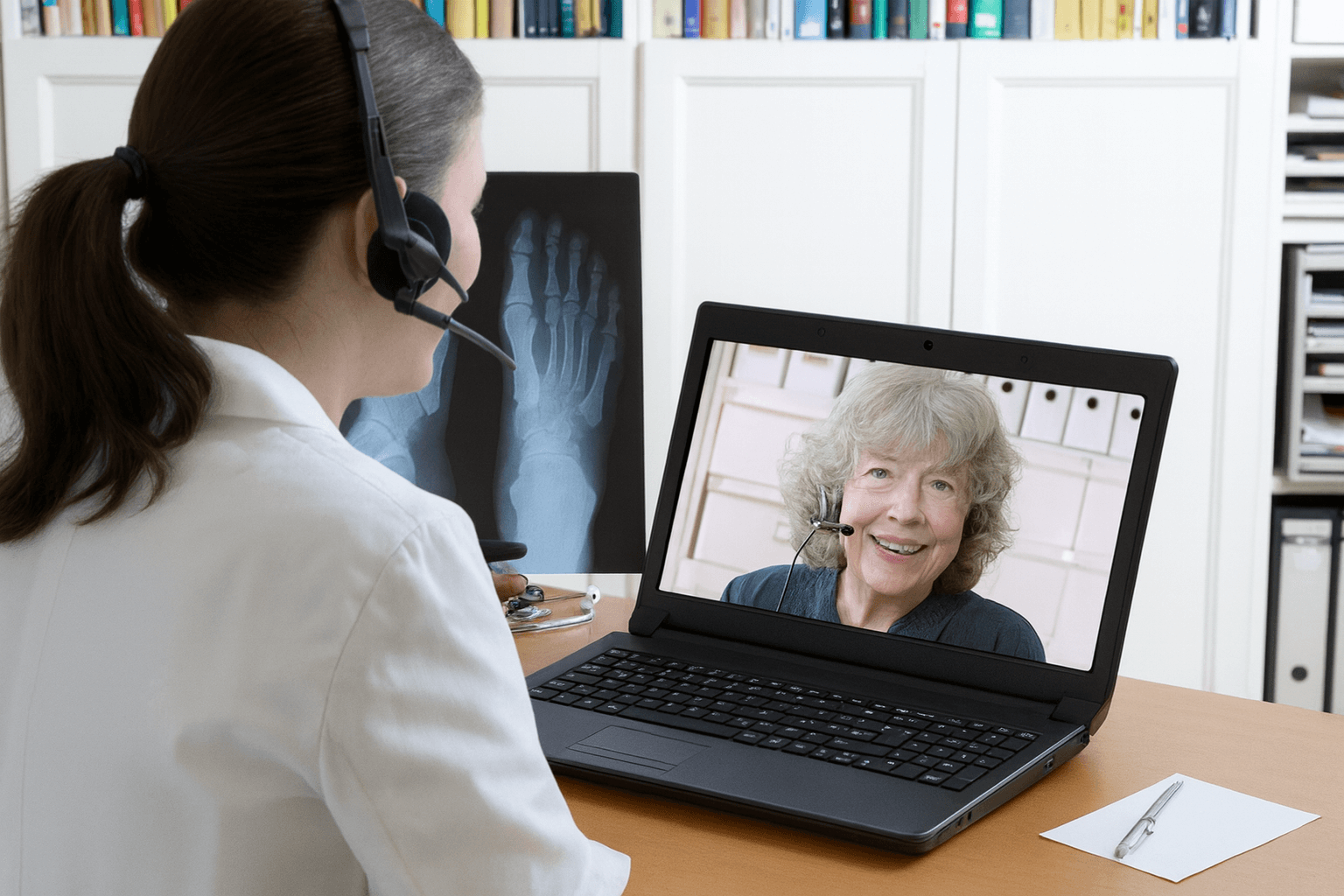
Remote triage allows trained professionals to assess symptoms, give clinical care advice, and direct patients to the right service before they reach a hospital or clinic.
The Veterans Health Administration has made remote triage a central feature of its care system. It is part of a larger shift toward digital health and telehealth services designed to improve access for all veterans. For adults seeking clinical care advice, remote triage serves as the first point of contact. It helps reduce delays, eases emergency room overcrowding, and promotes better patient outcomes.
Planning Remote Triage for Adult Care
Planning remote triage requires a strong foundation. Veterans Affairs research identified several themes that guide success. Staff training is one of the most important elements. Without proper training, protocols may be misapplied and safety may be at risk. Planning remote triage must include education, simulations, and continuing support.
Workplace environment and workload also matter. High stress or poor staffing ratios can reduce performance. Veterans Affairs studies emphasize the importance of well-being and manageable caseloads to sustain quality. Another factor is the triage system itself. Algorithms, clinical decision support tools, and workflows must be designed for consistency. Planning should also focus on integration with electronic health records. Without this, care continuity may be lost.
External factors influence planning as well. Veterans often live in rural areas or face barriers such as limited broadband access. Systems must adapt to these conditions to ensure all veterans have fair access to triage services. Successful planning means anticipating these challenges and building inclusive solutions.
What Are the Identified Best Practices for Execution
Execution is where planning meets reality. Best practices in execution begin with communication. Patients calling for advice may feel uncertain or anxious. Clear, empathetic communication builds trust and helps ensure that advice is followed. Veterans Affairs has invested in communication training to support safe interactions.
Safety is central. Protocols must trigger immediate escalation when high risk symptoms are identified. Clinical decision support tools guide staff but must be used with judgment. Execution triage strategy also benefits from variety. While telephone triage remains the most common, video and app-based tools provide more choice. Veterans Affairs continues to expand VA telehealth options to meet the needs of diverse patient groups.
Responsiveness is another core theme. Wait times must be minimized, and call surges must be handled with backup staff. Research shows that including nurse practitioners in triage centers can reduce unnecessary emergency visits. Their advanced skills strengthen decision-making, improve accuracy, and conserve resources.
Equity in execution ensures no veteran is left behind. Services should account for adults with disabilities, hearing loss, or limited digital literacy. Providing alternative options helps maintain fairness across the system.
Evaluation as a Continuous Learning Process
Evaluation ensures that remote triage systems improve over time. Veterans Affairs research stresses the need for measurement at every level. Metrics include call response times, accuracy of triage decisions, safety outcomes, and patient satisfaction. Evaluation of triage should also include downstream effects such as reduced emergency department visits and stronger follow-up with primary care.
Best practices highlight the value of feedback loops. Staff should receive regular feedback on performance, while leaders use data to refine protocols. Automated call recordings, data analytics, and integration with electronic health records make detailed evaluations possible.
Research also shows differences between local and regional triage models. Local models may resolve more calls on first contact, while larger systems deliver consistency across regions. Veterans Affairs balances both, using centralized protocols with local responsiveness.
Evaluation gaps remain. Studies call for more research on cost, technology comparison, and provider type effectiveness. Veterans Affairs recognizes that filling these gaps will help create stronger systems in the future.
Why Veterans Affairs Provides a Strong Model
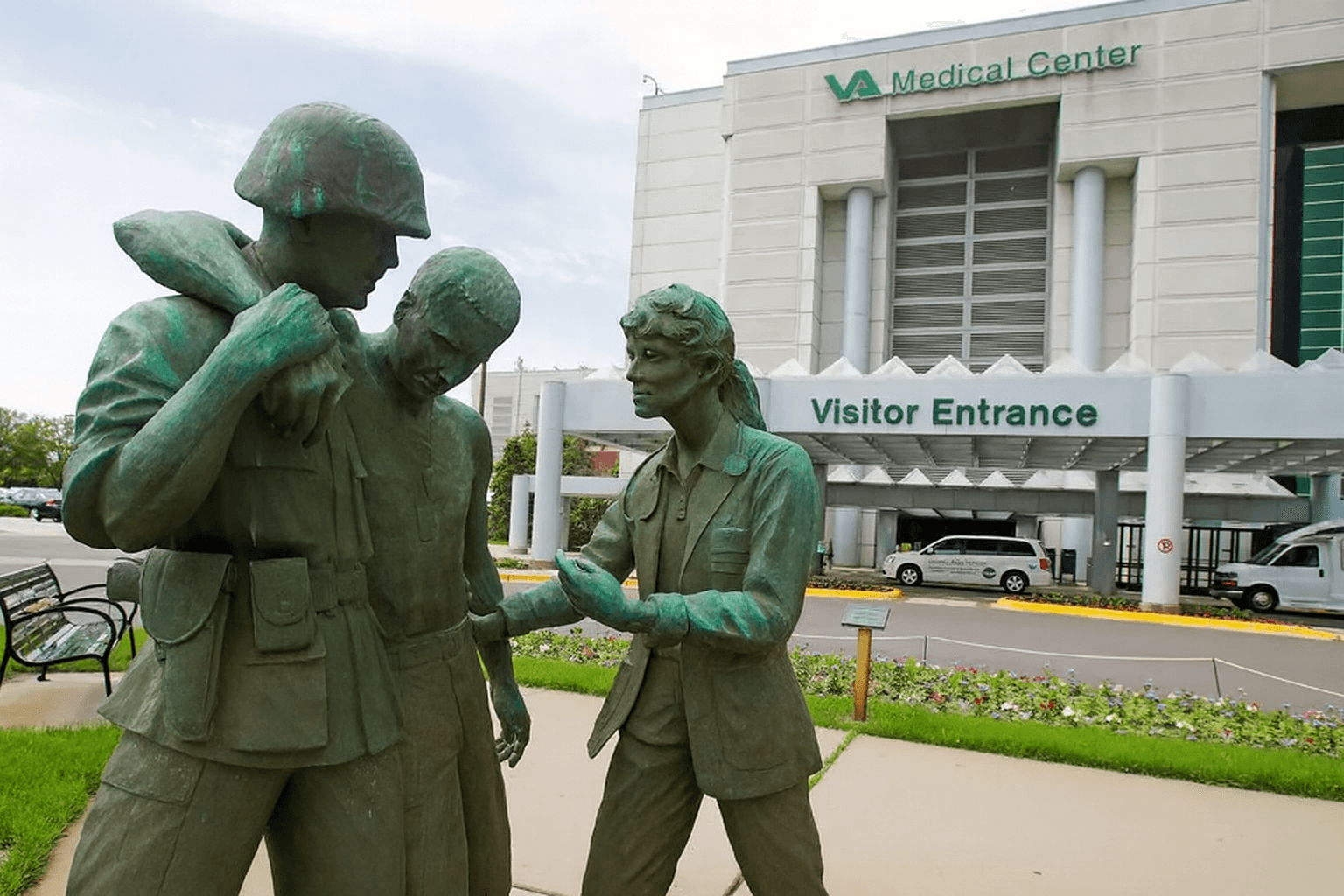
Veterans Affairs healthcare is one of the largest integrated health systems in the United States, serving millions of veterans through hospitals, clinics, and telehealth. Its approach to remote triage offers unique insights because of its scale and integration. Clinical Contact Centers provide 24/7 access, blending administrative and clinical support with standardized protocols.
Integration with electronic health records ensures that information from triage calls flows to the broader care team. This supports care continuity and reduces duplication. Veterans Affairs also invests in evidence-based tools, ensuring triage staff follow consistent pathways for safety.
VA telehealth demonstrates how large scale health systems can adapt to modern needs. By providing telephone, video, and digital pathways, Veterans Affairs improves access for rural patients and those unable to attend in-person visits. The scale of VA operations shows that remote triage can be both consistent and flexible.
Lessons for Large Scale Health Systems
While not all health systems match the size of Veterans Affairs, its best practices provide guidance. Planning should focus on training, staff support, and integrated systems. Execution must emphasize clear communication, equity, and responsiveness. Evaluation must be ongoing, using data to inform improvement.
Large scale health systems can also learn from the VA’s investment in multimodal telehealth. By offering choices, systems meet patients where they are and improve satisfaction. Veterans Affairs research proves that remote triage can support both efficiency and safety when done with thoughtful design.
Closing Insights for Health Leaders
Remote triage best practices involve more than quick decision-making. They represent a structured system that blends planning, execution, and evaluation into a cycle of improvement. Veterans Affairs research highlights themes such as staff training, well-being, technology integration, and patient-centered communication. These lessons apply across health systems and help ensure safe, effective care delivery.
As demand for timely clinical care advice grows, systems that adopt best practices in triage will be better prepared to meet the challenge. Veterans Affairs demonstrates that it is possible to provide consistent, reliable triage on a national scale while maintaining patient trust.
Apply lessons from Veterans Affairs to your own healthcare system. Build remote triage programs that combine planning, strong execution, and continuous evaluation to give patients safe and timely access to care.
