Strategic Roles Within Modern Healthcare Systems
Healthcare organizations operate under growing pressure to deliver high-quality care while maintaining compliance and financial balance. Each service must be reviewed for necessity and aligned with payer expectations. This system of checks and reviews is called Utilization Management, a structured process that keeps medical care effective, efficient, and compliant.
The function has become more complex as hospitals expand and data systems evolve. Internal teams handle thousands of authorizations, verifications, and documentation tasks each week. To maintain consistency and accuracy, hospitals now rely on specialized operational support systems that simplify Utilization Management and sustain performance across departments.
Why Utilization Management Needs Operational Support
Every healthcare institution recognizes the importance of proper Utilization Management, yet few have the internal bandwidth to manage it effectively. The process demands a blend of clinical judgment, data accuracy, and administrative coordination.
Manual documentation and outdated systems often slow down approvals. Missed details cause claim denials, compliance risks, and patient dissatisfaction. Without streamlined review structures, even the best medical programs face operational delays.
Healthcare networks need partners that can provide infrastructure and expertise without disrupting clinical care. These operational systems handle the complex, repetitive, and time-sensitive work that keeps reviews moving efficiently.
Integrated Review Systems in Healthcare Operations

Hospitals rely on strong internal systems to ensure that Utilization Management functions with speed and precision. These systems must adapt to the hospital’s workflow and maintain alignment between patient care, documentation, and compliance.
Through structured and data-driven frameworks, Care Agent BPO enables healthcare teams to manage every phase of Utilization Management effectively. From preauthorization to retrospective verification, each stage follows standardized rules to support accuracy and fairness.
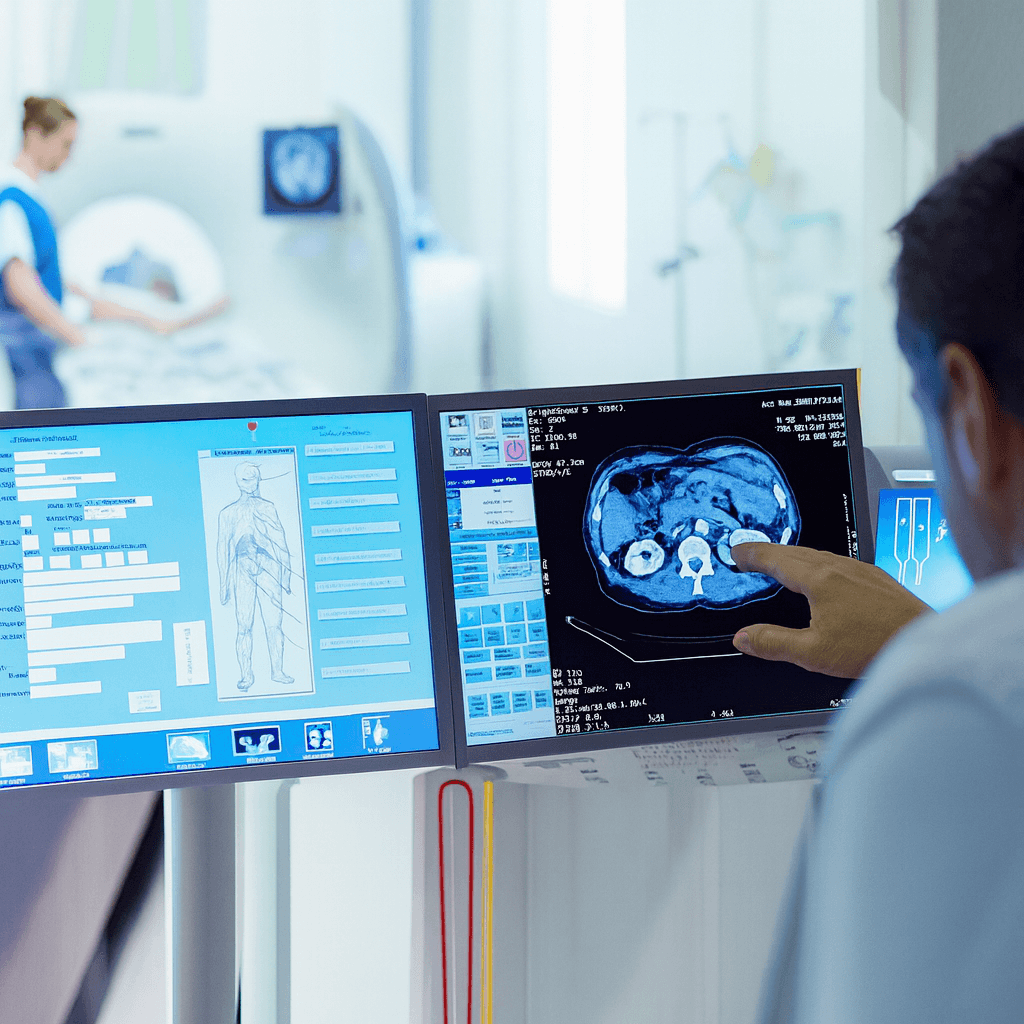
Automation tools streamline documentation, flag missing data, and reduce manual workload. Reviewers spend less time searching for information and more time evaluating medical needs. This integration of technology and expertise transforms Utilization Management from a reactive task into an active part of quality care.
How Digital Integration Strengthens Healthcare Systems
Technology now drives Utilization Management forward. Hospitals no longer depend solely on paper files or manual tracking systems. Secure cloud networks, analytics platforms, and real-time dashboards have replaced traditional tools, making operations faster and more transparent.
Integrated systems connect payers, physicians, and administrative teams. Data travels between them instantly, reducing miscommunication and accelerating approvals. Automated reminders and digital case logs keep each stage accountable.
This digital coordination saves time and lowers costs. It also ensures that every medical service is backed by evidence, review history, and proper documentation. Digital transformation is not just a convenience; it is a requirement for sustainable healthcare operations.
What Challenges Do Hospitals Face Without Integration
Without strong Utilization Management structures, hospitals risk inefficiency and financial strain. Uncoordinated workflows lead to inconsistent reviews, missed deadlines, and increased administrative load. These issues cause frustration across departments and create barriers between clinical and operational teams.
When approvals lag, patient treatments are delayed, and claims remain unresolved. Over time, the absence of automation and structured review systems weakens both compliance and care quality.
Healthcare systems that adopt integrated solutions experience immediate relief from these challenges. Digital tools track progress, standardize review formats, and document every action in real time. This consistency preserves resources while improving transparency for every stakeholder involved.
System Alignment and Long-Term Value Creation
Efficiency in healthcare depends on alignment, between clinical practice, policy, and operations. Utilization Management provides that link by verifying necessity and maintaining transparency across every phase of care.
Strong review frameworks also generate insight. Data gathered from Utilization Management helps hospitals identify usage trends, evaluate staff workloads, and forecast future service needs. This information supports better budgeting, resource allocation, and regulatory readiness.
Through consistent oversight, hospitals maintain stability even during volume surges or policy shifts. The process not only protects revenue but also ensures patient care remains timely and evidence-based.
Evolving Partnerships in the Healthcare Ecosystem
Healthcare systems now build extended partnerships to strengthen internal performance. These relationships combine technology, staffing, and analytics to sustain Utilization Management on a large scale.
Strategic partners supply specialized review teams who understand payer requirements and compliance demands. They manage the workflow from start to finish, ensuring that every authorization or appeal is processed correctly and efficiently.
By integrating with existing operations, these external systems expand capacity without creating disruption. Hospitals maintain clinical control while gaining scalable support that adjusts to demand. This model improves flexibility and allows leadership to focus on patient-centered goals.
The Future of Utilization Management in Healthcare
The next phase of Utilization Management will be defined by automation and predictive intelligence. Systems will anticipate trends, flag inconsistencies, and optimize approval routes before issues occur.
Human expertise will remain central, but technology will handle data verification and audit preparation. Predictive analytics will identify high-risk areas in resource use, allowing hospitals to act early. These improvements will transform Utilization Management from oversight to foresight.
Specialized systems like those built by operational service providers will remain essential. They will continue bridging gaps between compliance, efficiency, and patient satisfaction. Healthcare organizations that embrace these innovations today will set the new standard for tomorrow.
Strengthening Healthcare Through Intelligent Review Systems
Healthcare excellence depends on the ability to blend technology with clinical responsibility. Utilization Management embodies that balance by keeping patient care aligned with measurable standards.
Organizations that invest in modern systems see stronger compliance, faster approvals, and improved satisfaction across every department. Through structured operations, healthcare networks achieve consistency without sacrificing compassion.
As the healthcare environment continues to evolve, intelligent Utilization Management remains a cornerstone of sustainability. It protects patients, supports providers, and builds confidence in every decision made within the system.
